Overprescribed
Common painkillers can become a gateway to opioid addiction.
“I broke my nose playing basketball when I was 15 and I was prescribed tylenol-3’s, which are codeine. I remember I just took them and I liked the way they made me feel. It was a different high than weed, and when I put the two together it was exactly what I’d been looking for, so that started [my addiction]. If I put myself in my shoes while I was in high school, there was nothing anyone really could’ve said to stop me from doing what I was doing, because that just seemed so far from reality. If someone were to tell me that by the age of 21 I’d be shooting meth and heroin, I’d tell them like, ‘No that’s ridiculous, I just drink lean and smoke weed, I know my limits, I would never,’” said CHS graduate Jack Bernard.
Bernard’s experience with illegal substances began in middle school, when he first tried smoking marijuana and enjoyed the high that resulted from it. However, his drug use escalated after he was prescribed opioids at the age of 15 and discovered that the euphoric feelings produced by this medication were preferable to those generated by the THC in marijuana. Throughout the following six years, Bernard spent copious amounts of time and money searching for his next high, which, he contended, was not very difficult to find.
“I had multiple dealers, I already knew where to get these drugs, and it wasn’t too hard. Honestly you could drive into the city and find them on just about every corner of a bad neighborhood. But it wasn’t tough. I was broke all the time. It continued for years,” Bernard said.
Substance addiction put considerable strain on Bernard’s relationships with friends and family. Even those that he got high with began to worry for his health and safety.
“People told me to stop all the time, there were all the warning signs. Like even my close friends, even the people I got high with in high school were telling me to stop, you know. And it’s like, when the people you get high with are telling you that you have a problem then you probably have a problem,” Bernard said.
Bernard began to seek out treatment when he realized that his substance addiction controlled his life and sidetracked him from his ambitions.
“I was just doing really bad and I had been introduced to recovery on and off for a while,” Bernard said. “I mean I didn’t just go to treatment one time and get better, I had been in and out of treatment centers for two years, so I already knew it was out there and I was in a really bad place at the time. I never had any money, I was always sick, I didn’t really have any relationships with friends or family. My life sucked. I didn’t really have anything to live for. That’s when I reached out for help and started down this path of recovery.”
Currently, Bernard works as a director of operations for a string of sober living facilities in Austin, Texas, a job which was offered to him after recovering in the facilities himself. Sobriety has allowed Bernard to live a less chaotic life and to rebuild relationships with those close to him.
“For my family, it was a very strained relationship when I was getting high. Now that I’m sober, it’s better than it ever has been,” Bernard said.
To current high school or college students, Bernard cautioned against experimentation with drugs, especially because of their degenerative effects on the brain during such a crucial period of growth. Yet, he also stressed the fact that substance use of some kind is normal in teens, and does not always lead to long-term negative consequences.
“I mean, it’s tricky, because not everyone who does these drugs is going to get addicted,” Bernard said. “Like someone in high school could take the xanax or opioids or whatever it may be and they could go to a party, have fun, and wake up the next morning and do their homework and go to school on Monday. But there are some people who can’t control it, like they’ll go out and have a few drinks and go do some coke. Or take some xanax and then have to keep doing it and feel like they have to keep taking more and more and more. That’s what separates the addict from the normal user. It’s not abnormal to use drugs and drink alcohol. That’s not something that’s necessarily wrong to do either, in my opinion. Most kids under 21 have taken a drink or a drug; it’s just the fact of the matter. Not everyone is going to become an addict, but if I did have something to say I’d want it to reach that 10 percent who does.”
As a recovered addict, Bernard feels that his genetic predispositions and neurochemistry would’ve led him to substance abuse with or without the opioid prescription that he received at the age of 15. Yet, he also contended that those medications were not necessary to manage his pain. For the few teens with a similar predisposition, prescription opioids could act as a gateway for more destructive drug use.
CHS AP Biology teacher, Adam Bergeron, has had his own experience with opioids. He was prescribed the medication after an accident that occurred in his own classroom.
“I was here at school,” Bergeron said. “It was the day of the eclipse in 2017. I was in the prep room, right next to my classroom, preparing some materials for a lab experiment inside of a pressure cooker. I grew impatient; I did not wait for the pressure cooker to vent pressure appropriately. I began to open the release valves and liquid that was above the boiling point of water quickly escaped out of the pressure cooker and landed on my arms, and my back and my face and just about instantly caused second and third degree burns all across those parts of my body.”
Instead of rushing straight to the emergency room, the injured teacher waited the whole day before seeking medical attention.
“The long story short, I stayed here at school the entire day, stupidly, and went to an urgent care after school. Urgent care checked me out and told me to go to the emergency room. I went to the emergency room and that night I left with a small prescription––about 15 pills––to get me to an appointment with a dermatologist. I believe that opioid was Oxycodone, which is a combination of oxycontin and acetaminophen,” Bergeron said.
With his background in biology and science, Bergeron was wary of the highly addictive pain medication that had been prescribed to him.
“I had a pretty deep seated fear of the molecules, of these medicines,” Bergeron said. “I was very hesitant to take any of it, unless I knew I was going to sleep. At this point, that night and a couple days in, I was incredibly uncomfortable. I couldn’t roll over to my right side, which is usually where I sleep. My wife is a nurse practitioner and she made it clear that these medicines would help me sleep. I think I took one every thirty minutes before I would go to bed.”
Additionally, he refrained from taking the opioids during the day. Instead, he chose to ingest lower risk, over-the-counter pain medicine.
“I didn’t usually feel like I was in pain during the day. If I was uncomfortable, I would just take ibuprofen.”
Despite taking this strong medicine, Bergeron found himself without any addiction to Oxycodone.
“I never noticed a dependence [on the opioids],” said Bergeron. “The only dependence I can begin to describe was when I did go to see the dermatologist, and he recommended that I had to shave my arm where the burn took place. Because that skin was so new and so sensitive, the idea of scraping a razor across it would be incredibly painful. The dependency came in where before I attempted that, I had to take the medicine before. Again, about thirty minutes prior and before I went to bed. Otherwise that task would’ve been incredibly unmanageable.”
He was able to use the potentially dangerous and potent drugs carefully and as needed. This is usually the case––but not for all.
According to Washington University Professor of Emergency Medicine and Barnes Jewish Hospital Section Chief of Medical Toxicology Evan Schwarz, opioid prescription is unlikely to lead to addiction in most people. However, he additionally pointed out that for those with a genetic predisposition to an addictive personality, these drugs can cause a euphoric feeling that leads to that small percentage of users becoming dependent on opioids.
“Generally [addiction to opioids] starts with some type of exposure and the person really likes the feeling that they get from it. And they start using it more and more and more. With opioids especially you develop a tolerance, so you have to use more to get that type of euphoric feeling. Then over time there’s some changes that occur in the brain that cause a shift from the person feeling normal and using the drugs to get high and euphoric to using the substances so that they just don’t feel bad anymore. In particular with opioids, they’re using because they now feel very depressed and the only way that they can start feeling normal is by using. With opioids above other things they keep using because they don’t want to experience the symptoms of withdrawal,” Schwarz said.
Although it is difficult to determine who might be more susceptible to opioid addiction, there are tangible steps that can be taken to prevent patients from becoming reliant on their pain medications, especially teens. Opioids should only be taken for the minimum amount of time possible, and within that time-frame patients can attempt to ease pain with Tylenol or ibuprofen before turning to their prescription.
Additionally, parents with teens should pay close attention to their child’s consumption of prescribed opioids and make sure to dispose of any extra pills as promptly as possible.
“Especially talking about a patient who is under 18, the parents should be very involved in all of these types of things and they can also make sure that they’re monitoring very closely how many pills are being taken,” Schwarz said. “There was legislation that was passed this year in Missouri that a lot of pharmacies are required to take back the pills. There are also little disposal kits that you can get at pharmacies to get rid of extra pills. You can’t just throw them in the trash because then anyone could just pick them up out of the trash. There are also national take-back days for patients to get rid of any extra medication.”
The overprescription and disposal of these opioids is another problem that needs to be addressed. 40.5 percent of people who misused prescription pain relievers in 2015 reported that they got the drugs from a family member or friend who had the unused medicine on hand.
After all of this time, Bergeron still has a large quantity of his opioid prescription, despite no longer having a need for it.
“It’s over a year later and I still have two prescriptions. One for Oxycodone and one for a slightly higher dose of Oxycodone. They still sit in the drawer where I keep all of my toiletries. I asked my wife, ‘Can you bring these into your office so we can dispose of them?’ and she said, ‘Well, we can put them in the sharps box where needles and syringes go.’ She also shared with me that you can bring them to a police station or a fire stations and there’s ways to have them disposed of. I have not gone to that level of doing it. Other than an extreme headache about two months ago now, I haven’t opened that bottle, and I still have 30 or 40 [pills]. In terms of overprescribing, if you can handle the pain and you don’t take all of the medicine, you’re left with a lot of medicine. And what do you do with it when you have the extra medicine?”
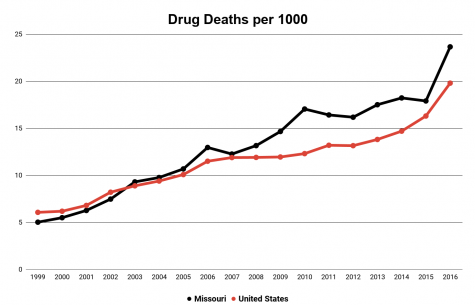
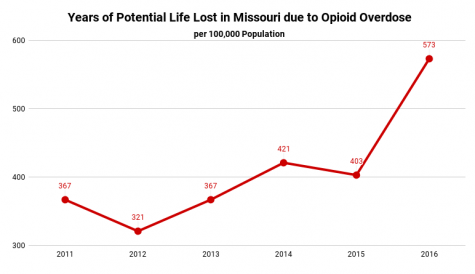
1 out of every 65 deaths in Missouri were due to opioid overdose.
Data sourced from the Missouri Department of Health and Senior Services.
This excess of medicine trickles down into the system of drug misuse. But what or who is responsible for opioids taking hold in society?
“There’s clearly some evidence that the manufacturer of these medicines advocated for their prescriptions and rewarded physicians who prescribe them. We have, as a society, really bad pain medicine. We don’t really fully understand pain. We understand the molecular basis of pain. But because pain is subjective, what one person experiences can be entirely different from what another person experiences. My wife can attest to that fact. When she meets with patients and they say they’re in pain, it’s one of the hardest things she has to chart. I think a lot of physicians have over prescribed these medicines because it’s better to be safe than sorry. It’s better to alleviate and treat, rather than leave somebody miserable and in pain,” Bergeron said.
“We are in dire need of medicine that works, is less likely to be abused, but is still available to people who need it.”
A $50 or more donation includes a subscription to the Clayton High School Globe 2024-2025 print news magazine.
We will mail a copy of our issues to the recipients of your choice.
Your donation helps preserve the tangible experience of print journalism, ensuring that student voices reach our community and that student democracy thrives.
Grace Snelling is a senior and is Editor-In-Chief of the Globe this year. She has previously been a reporter, page editor, and senior managing editor. Throughout her childhood,...

Lila is a junior and this is her third year as a member the Globe staff. She is a senior managing editor and is very excited for the year ahead. She was a feature section editor...












Maureen McDonald • Nov 10, 2018 at 9:07 am
I appreciate the depth and breath of this article. Interviewing a couple different people who received pain medication, and illustrating the differences in how they used itWho is very effective. I appreciate it the health department shirts, though the data is very sobering. Thank you to the others for a thorough job on an important topic.